What Is the Motor End Plate? Your Essential Guide to Muscle Communication and Function
Table of contents
- Introduction: The critical link between nerve and muscle
- Defining the motor end plate (MEP): A specialized neuromuscular synapse
- Core definition
- Location and purpose
- Synonymous terms
- Anatomy of the motor end plate: Structures for signal transmission
- The presynaptic terminal (nerve side)
- The synaptic cleft (the gap)
- The postsynaptic membrane (muscle side)
- How the motor end plate works: The mechanism of muscle activation
- Nerve impulse arrival
- Acetylcholine release
- Receptor binding and depolarization
- End plate potential (EPP) generation
- Muscle action potential
- ACh inactivation and recovery
- Link to contraction
- Miniature end plate potentials (MEPPs), quantal release, and synaptic delay
- Clinical significance: When motor end plate function goes awry
- Myasthenia gravis (MG)
- Lambert-Eaton myasthenic syndrome (LEMS)
- Botulism
- Organophosphate poisoning
- Other toxins and pharmacology of neuromuscular blockers
- Diagnosis and management of MEP disorders
- Diagnostic methods
- Treatment strategies
- Growth, repair, and plasticity at the motor end plate
- Quick comparisons and FAQs I get from students
- Conclusion: The orchestrator of our every move
Introduction: The critical link between nerve and muscle
The first time I watched a muscle twitch on an oscilloscope after a nerve stimulus I felt like I had peeked behind the curtain of everyday life. You decide to lift your coffee mug. Your forearm flexors contract like it is the simplest thing in the world. Under the hood a beautiful conversation happens between a motor neuron and a skeletal muscle fiber. The place they meet has a name that sounds small yet carries huge weight for movement. That place is the motor end plate.
In my experience, everything clicks when you treat the motor end plate as a purpose‑built interface. It sits at the neuromuscular junction, it translates a motor nerve impulse into a muscle action potential, and it starts the chain of events that ends in muscle contraction. No motor end plate, no voluntary movement. Simple as that.
I like a good analogy. When I explain this to engineering‑minded friends I compare the neuromuscular junction to a precision electromagnetic machine. Engineers fine‑tune magnetic pathways with layered metals to reduce losses and boost signal fidelity. That design mindset mirrors how biology packs ion channels and junctional folds at the motor end plate to focus current and trigger contraction. If you have ever read about electrical steel laminations or the role of a stator core lamination you have felt the same spirit of smart signal transfer that the motor end plate embodies.
Defining the motor end plate (MEP): A specialized neuromuscular synapse
Core definition
Here is the clean definition I use with students. The motor end plate is the specialized region of a skeletal muscle fiber’s membrane that forms a synapse with the axon terminal of a motor neuron. It is the postsynaptic side of a neuromuscular junction built to capture acetylcholine and convert chemical signals into electrical depolarization.
Location and purpose
You find motor end plates on skeletal muscle fibers. Not on smooth muscle. Not on cardiac muscle. A single alpha motor neuron branches to innervate multiple fibers which together form a motor unit. Each branch ends on a specific patch of the sarcolemma that looks different under a microscope. That patch is the motor end plate. Its singular job is simple yet profound. It receives acetylcholine from the nerve terminal, depolarizes the muscle membrane, and if the depolarization is strong enough it launches a muscle action potential that travels across the sarcolemma and down the T‑tubules to trigger contraction.
Synonymous terms
You may hear people use “motor end plate” and “neuromuscular junction” interchangeably. I separate them. The neuromuscular junction (NMJ) includes the presynaptic terminal, the synaptic cleft, and the postsynaptic membrane. The motor end plate is the postsynaptic membrane and its substructures. That distinction keeps the anatomy tidy in my head.
Anatomy of the motor end plate: Structures for signal transmission
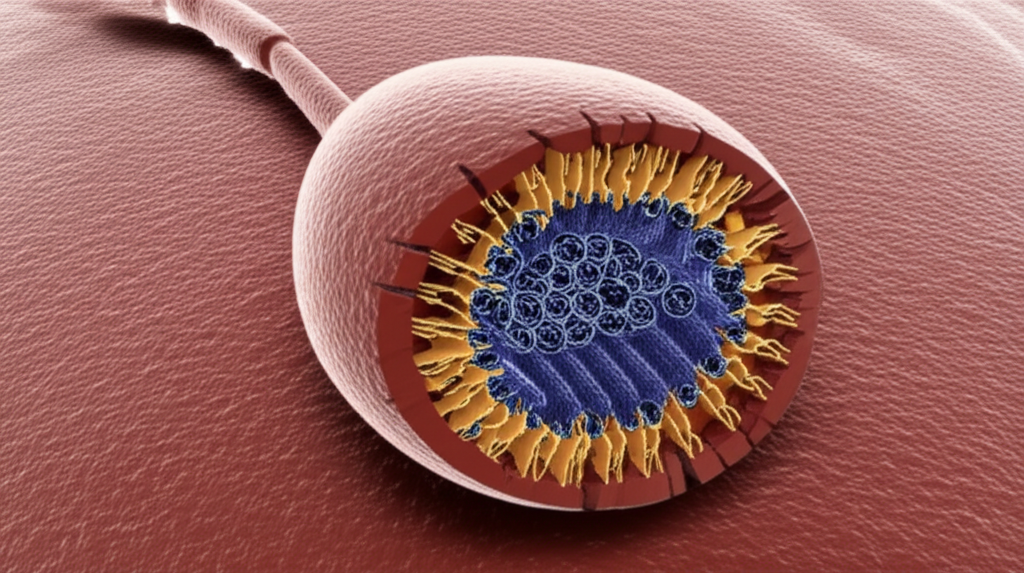
The motor end plate works because its structure funnels current like a well‑designed waveguide. Let me walk you through the main parts from nerve to muscle.
The presynaptic terminal (nerve side)
- Axon terminal: The myelinated motor axon loses its myelin near the end then flares into a terminal bouton that nestles in a shallow depression of the muscle fiber. Schwann cells cap the terminal and help maintain the microenvironment.
- Synaptic vesicles: The terminal bouton packs small vesicles loaded with acetylcholine (ACh). Vesicles cluster near active zones that face the muscle membrane.
- Voltage‑gated calcium channels: When a motor neuron action potential invades the terminal these channels open. Calcium ions rush in and drive vesicle fusion. That calcium trigger is the heartbeat of synaptic transmission at the NMJ.
The synaptic cleft (the gap)
- The cleft: A narrow extracellular space separates nerve and muscle. The architecture minimizes diffusion distance but still leaves room for critical proteins.
- Basal lamina: A specialized extracellular matrix coats the cleft. It positions enzymes and adhesion molecules. One celebrity here is acetylcholinesterase.
- Acetylcholinesterase (AChE): This enzyme waits in the cleft like a cleanup crew. It hydrolyzes acetylcholine into acetate and choline which terminates the signal fast. Without AChE the signal lingers which causes chaos.
The postsynaptic membrane (muscle side)
- Sarcolemma with junctional folds: The motor end plate is not smooth. It forms deep junctional folds or subneural clefts. These folds multiply surface area and slot ion channels exactly where they are needed.
- Nicotinic acetylcholine receptors (nAChR): These ligand‑gated ion channels cluster at the peaks of the junctional folds. ACh binding opens them which allows mainly sodium influx and some potassium efflux. The result is a depolarizing current.
- Voltage‑gated sodium channels: You find a high density of these at the depths of the folds and around the perijunctional zone. They take the small depolarization caused by nAChR opening and turn it into an all‑or‑none muscle action potential.
When I first saw an electron micrograph of the motor end plate the logic of those folds hit me. Biology solved the same physics problem we face in electronics. How do you keep a small current from fizzling out. You pack receptors and downstream sodium channels tightly in a corrugated landscape. The local current has nowhere to hide.
How the motor end plate works: The mechanism of muscle activation
The choreography at the motor end plate runs fast. Yet each step follows a reliable script. Here is the sequence I teach and test myself on when I need a quick refresher.
Nerve impulse arrival
An action potential travels down the alpha motor neuron. Myelination speeds conduction along the axon which belongs to the somatic nervous system. As the impulse reaches the terminal bouton it loses myelin which slows it a hair and shapes the action potential that the terminal sees.
Acetylcholine release
The arriving action potential depolarizes the terminal. Voltage‑gated calcium channels open and calcium flows into the nerve terminal down its electrochemical gradient. Calcium binds to vesicle fusion machinery. Vesicles fuse with the membrane at active zones which causes exocytosis of ACh into the synaptic cleft.
Receptor binding and depolarization
Acetylcholine diffuses across the cleft in a blink. It binds to nicotinic ACh receptors concentrated at the crests of the junctional folds. These ligand‑gated channels open which allows sodium ions to rush in and a smaller amount of potassium to move out. The local membrane depolarizes. That depolarization is the end plate potential.
End plate potential (EPP) generation
The end plate potential is graded which means bigger ACh release makes a bigger EPP. At a healthy motor end plate a single nerve impulse releases enough ACh to produce an EPP that exceeds threshold. Redundancy is built in which keeps movement reliable even as conditions vary.
Muscle action potential
If the depolarization reaches threshold voltage‑gated sodium channels along the folds and perijunctional zone open. The signal becomes regenerative. A muscle action potential launches and propagates along the sarcolemma then dives into the T‑tubules. That propagation recruits the entire muscle fiber.
ACh inactivation and recovery
Acetylcholinesterase in the basal lamina splits ACh into acetate and choline. That reaction shuts the gate on the nAChR which stops the end plate current. The presynaptic terminal retrieves choline by a high‑affinity transporter. It uses choline acetyltransferase to resynthesize ACh then refills vesicles. Vesicle membrane gets recycled by endocytosis pathways that keep the terminal supplied for the next volley.
Link to contraction
The muscle action potential triggers excitation‑contraction coupling. Dihydropyridine receptors in T‑tubules sense the voltage change then talk to ryanodine receptors in the sarcoplasmic reticulum. Calcium floods the cytosol which lets actin and myosin interact. The fiber shortens. You lift the mug with barely a thought.
Miniature end plate potentials (MEPPs), quantal release, and synaptic delay
A few details always fascinate me because they reveal the NMJ’s precision.
- MEPPs: Even when the motor neuron is quiet you can record tiny depolarizations at the motor end plate called miniature end plate potentials. Each MEPP represents the effect of one vesicle’s worth of ACh released spontaneously. They prove that transmitter release is quantal.
- Quantal release: Vesicles are the currency of communication at the NMJ. A nerve impulse increases the probability that many vesicles will fuse at once which stacks their quanta of ACh into a big EPP. This property explains the stepwise distribution of EPP sizes you see in careful experiments.
- Synaptic delay: There is a brief delay between nerve action potential arrival and the muscle response. Most of that delay comes from the time required for calcium to trigger vesicle fusion and for ACh to diffuse and bind. The delay is short yet measurable. In a system that controls movement milliseconds count.
Clinical significance: When motor end plate function goes awry
Every year I meet someone who has learned these concepts the hard way. A drooping eyelid that gets worse at the end of the day. A patient who cannot hold a smile. A farmer exposed to pesticides who develops muscle fasciculations then respiratory distress. These stories start at the motor end plate.
Myasthenia gravis (MG)
- Pathophysiology: Myasthenia gravis is an autoimmune disease that targets the postsynaptic membrane usually by antibodies against acetylcholine receptors. Receptor numbers drop and the junctional folds flatten. The EPP shrinks below threshold more often which produces fatigable weakness. Some patients have antibodies against other postsynaptic proteins which disrupts the same process.
- Symptoms: Fluctuating muscle weakness that worsens with use and improves with rest. Classic signs include ptosis, diplopia, trouble chewing or swallowing, dysarthria, and proximal limb weakness. Respiratory muscles can fail which creates a myasthenic crisis.
- Treatment snapshot: Cholinesterase inhibitors like pyridostigmine or neostigmine improve transmission by increasing ACh in the cleft. Immunosuppressive therapy such as prednisone, azathioprine, or mycophenolate mofetil reduces antibody production. Some patients benefit from rituximab or eculizumab. Thymectomy helps selected cases. In severe exacerbations IVIG or plasmapheresis buys time while longer‑acting therapies take effect.
Lambert‑Eaton myasthenic syndrome (LEMS)
- Pathophysiology: LEMS hits the presynaptic side. Autoantibodies target voltage‑gated calcium channels on the motor nerve terminal. Calcium entry falls and vesicle release falters. The result is a small EPP despite intact receptors on the muscle.
- Symptoms: Proximal muscle weakness that often improves with brief exercise. Autonomic symptoms can show up such as dry mouth or constipation. LEMS can occur as a paraneoplastic syndrome which is commonly associated with small cell lung cancer so a cancer search matters.
- Treatment snapshot: Treat any underlying cancer. Immunotherapies help like they do in MG. Agents that boost presynaptic release sometimes help. Repetitive stimulation can transiently increase strength due to brief facilitation at the synapse.
Botulism
- Mechanism: Botulinum toxin cleaves SNARE proteins required for vesicle fusion. The presynaptic terminal cannot release acetylcholine. The postsynaptic side sits ready yet silent.
- Symptoms: Bulbar weakness often appears first with diplopia, dysphagia, and dysarthria. Descending flaccid paralysis can follow. Respiratory failure is the fear.
- Notes: Botulinum toxin is infamous yet it is also a precise therapeutic tool when applied locally to reduce spasticity or cosmetically to relax muscles. Context and dose define its character.
Organophosphate poisoning
- Mechanism: Organophosphates irreversibly inhibit acetylcholinesterase. ACh floods the synaptic cleft and overstimulates nicotinic and muscarinic receptors. That storm causes initial muscle fasciculations followed by depolarization block and paralysis.
- Symptoms: The cholinergic crisis picture includes salivation, lacrimation, urination, diarrhea, gastrointestinal cramping, emesis, miosis, bradycardia, bronchorrhea, bronchospasm, and skeletal muscle weakness. Nerve gases like sarin act through the same pathway which underscores the seriousness.
- Treatment snapshot: Immediate decontamination and airway management matter most. Atropine counters muscarinic effects. An oxime like pralidoxime can reactivate AChE if given before the enzyme “ages.”
Other toxins and pharmacology of neuromuscular blockers
- Curare and non‑depolarizing blockers like rocuronium sit on the nAChR without opening the channel. They block transmission and produce flaccid paralysis during anesthesia which allows safe intubation and controlled surgery.
- Depolarizing blockers like succinylcholine bind and open the receptor which causes sustained depolarization then desensitization. The initial fasciculations followed by paralysis reflect that two‑phase action.
- Alpha‑bungarotoxin binds irreversibly to nicotinic receptors which makes it a powerful lab tool to label AChRs in research.
- Tetanus toxin is different. It does not target the motor end plate. It blocks inhibitory neurotransmission in the central nervous system which causes spastic paralysis. A helpful contrast when you study neurotoxins.
When you frame each disease by which side of the synapse it hits the patterns make sense. Presynaptic failure like LEMS means poor transmitter release. Postsynaptic failure like MG means the signal arrives yet the receptor landscape cannot capture it. Enzyme failure like organophosphate poisoning means the signal never shuts off.
Diagnosis and management of MEP disorders
When I help a learner think through a suspected NMJ problem we start with this checklist. What is the clinical picture. What tests confirm the target. What treatments fix the mechanism.
Diagnostic methods
- Electromyography (EMG) and nerve conduction studies (NCS): Routine EMG can show a decremental response on low‑frequency repetitive nerve stimulation in MG. LEMS often shows facilitation with high‑frequency stimulation or after exercise. Single fiber EMG is highly sensitive and detects increased jitter due to transmission variability at the NMJ.
- Antibody testing: Anti‑AChR antibodies support MG. Anti‑voltage‑gated calcium channel antibodies support LEMS. These tests add weight to a clinical diagnosis but you do not treat a lab test you treat the person in front of you.
- Pharmacologic tests: Historically the edrophonium test offered quick improvement in MG due to transient cholinesterase inhibition. Safer bedside tests use ice packs for ptosis or observe response to pyridostigmine under supervision.
Treatment strategies
- Cholinesterase inhibitors: Pyridostigmine is a mainstay for MG symptom control. By slowing ACh breakdown it boosts the end plate potential without changing the underlying autoimmune process.
- Immunosuppression: Prednisone helps many patients quickly. Steroid‑sparing agents such as azathioprine or mycophenolate mofetil maintain control long term. Biologics like rituximab or eculizumab may be indicated in selected cases.
- Rapid immunomodulation: IVIG and plasmapheresis offer short‑term improvement which helps in crises or preoperatively.
- Surgical: Thymectomy benefits appropriate MG patients especially with thymic pathology.
- Supportive care: Monitor respiratory function because diaphragm and accessory muscles tire. Early ventilatory support saves lives. Educate patients about medications that can worsen NMJ transmission such as certain antibiotics or magnesium.
I keep a simple rule of thumb. If the problem is weak receptor activation consider boosting ACh. If the problem is immune destruction turn down the immune attack. If the problem is toxin binding remove or counter the toxin then support the patient until the synapse recovers.
Growth, repair, and plasticity at the motor end plate
The motor end plate is not a fixed monument. It adapts as life unfolds.
- Denervation sensitivity: When a muscle fiber loses its nerve supply it sprouts ACh receptors across the entire sarcolemma not just at the end plate. This change increases sensitivity to ACh and sets the stage for reinnervation.
- Reinnervation: Surviving motor axons can sprout collaterals that reinnervate denervated fibers. New synapses form and the receptor field shrinks back to the end plate region. Strength returns although fine control may differ.
- Neurotrophic factors: Molecular signals guide this dance. They shape receptor clustering and maintain junctional folds. You do not need to memorize every molecule to appreciate the big idea. Structure follows function in both directions.
- Synaptic plasticity: Frequency of use changes transmission probability. Short‑term facilitation or depression can appear with different stimulation patterns. These dynamics show up during repetitive nerve stimulation studies that clinicians use for diagnosis.
I love pointing out that these biological upgrades echo the way engineers iterate electric machines. They add laminations to transformers to tighten magnetic pathways. They tweak motor core laminations to reduce losses and improve efficiency. Muscle and nerve refine their junctions for the same reason. Better signal. Better performance.
Quick comparisons and FAQs I get from students
- Is the motor end plate the same as a sensory structure like a muscle spindle or Golgi tendon organ? No. The motor end plate is a motor synapse on skeletal muscle. Muscle spindles and Golgi tendon organs are sensory receptors that report stretch or tension back to the nervous system.
- Which motor neurons form motor end plates. Alpha motor neurons innervate extrafusal skeletal muscle fibers and create classic motor end plates. Gamma motor neurons innervate intrafusal fibers inside muscle spindles which serve a different role.
- Are there sodium and potassium channels at the motor end plate beyond the nicotinic receptor. Yes. The nAChR is a ligand‑gated cation channel that carries most of the depolarizing current via sodium influx. Voltage‑gated sodium channels at the depths of the folds amplify that depolarization into a muscle action potential. Potassium channels help repolarize the membrane afterward and shape excitability.
- What about synaptic delay. The NMJ is fast but not instantaneous. Calcium entry and vesicle fusion take a sliver of time. Diffusion adds a hair more. The result is a brief and reliable delay between nerve signal and muscle response.
- Is there neurotransmitter reuptake. Acetylcholine itself is hydrolyzed rather than taken back up intact. Choline gets reuptaken by the presynaptic terminal and recycled to make new ACh. Endocytosis retrieves vesicle membrane to keep the release machinery stocked.
Conclusion: The orchestrator of our every move
When I strip away the fancy terms I picture the motor end plate like a tiny stage built for a single act. A nerve arrives with a spark. The stage lights flare as acetylcholine opens receptor channels. The set design funnels current down junctional folds where sodium channels stand ready. The spark becomes a wave. Calcium pours out of the sarcoplasmic reticulum. The muscle fiber bows and moves.
That single performance repeats across millions of fibers as you smile or sprint or write your name. The motor end plate sits at the heart of voluntary movement. It balances power with precision. It handles noise with redundancy. It adapts when life changes.
You do not need to memorize every protein to respect what happens here. Remember the three parts. Presynaptic terminal with vesicles and voltage‑gated calcium channels. Synaptic cleft with acetylcholinesterase and basal lamina. Postsynaptic membrane with junctional folds and nicotinic receptors. Understand the flow. Action potential to calcium entry to ACh release to receptor opening to end plate potential to muscle action potential to contraction. Then consider what breaks. Autoimmune attack on receptors, calcium channels blocked by antibodies, vesicle release shut down by toxins, enzyme inhibition that drowns the synapse in ACh.
If you ever feel lost come back to the core picture. The motor end plate is a specialized patch of muscle membrane that converts a chemical message into an electrical impulse. That impulse makes movement possible. The rest are details which you can learn at your pace with patience and practice.
And if analogies help you like they help me keep in mind how engineers shave losses and sharpen signals with laminated cores in motors and transformers. They are solving the same puzzle by different means. Biology uses folds and channels instead of steel and varnish. The goal is the same. Clean energy transfer with minimal waste.
I hope this walk‑through leaves you with a clear mental model. The next time your eyelid blinks or your hand steadies a cup you will know the quiet star behind the motion. The motor end plate took the call and delivered the message without missing a beat.